Congratulations to all of our 2025 APAMSA Research Award winners!
Be sure to stay tuned for more opportunities to feature your research at upcoming regional and national conferences.
Interested in featuring your research with APAMSA? Email research@apamsa.org for more information!
Research Award Winners
Anne Chen – Impact of a Community Stroke Education Initiative for the Nashville Asian American and Pacific Islander Population
Background: Prior studies demonstrate an increased prevalence of primary intracranial hemorrhage with lengthened hospital stays within the Asian American and Pacific Islander (AAPI) population. AAPI patients who experience acute ischemic strokes may be less likely to receive intravenous thrombolytic therapy despite presenting with strokes of greater severity.[1] Yet, minimal research has been conducted to explore why these disparities exist. This project was conducted to assess for gaps within stroke education (symptom identification, risk factors, and primary prevention measures) and evaluate the utility of a stroke outreach initiative in the Nashville AAPI community.
Methods: A stroke outreach initiative was designed and administered to provide education on stroke symptoms using the FAST acronym, risk factors, and the importance of regular follow-up with primary care. Participants also received stroke educational materials in English, Simplified Chinese, Japanese, Korean, or Vietnamese from reliable sources (e.g., the American Heart Association, MedlinePlus). Pre- and post-education surveys assessed knowledge of stroke symptoms and primary stroke prevention. Proportional analysis and non-parametric analysis of paired comparisons (McNemar test) are reported.
Results: Twenty-two API community members at an AAPI festival in Nashville, TN participated in the initiative. Pre-initiative surveys revealed 8/22 (36%) participants were unable to identify stroke symptoms, 9/22 (40%) participants did not know what actions to take if someone is experiencing a stroke, and 10/22 (45%) participants did not follow up with primary care at least yearly (Figure 1). Post-initiative surveys showed a statistically significant improvement (p<0.05) where 21/22 (95%) participants correctly reported two of the FAST symptoms (Figure 2). 8/8 (100%) participants who previously were unable to identify stroke symptoms identified at least two symptoms post-initiative. All participants found this initiative beneficial.
Conclusion: An education initiative reviewing FAST symptoms, stroke risk factors, and primary stroke prevention through regular follow-up with primary care can improve the quality of stroke education in the Nashville AAPI population. Additional instruction and increased frequency of the initiative may improve retention of knowledge and further encourage stroke awareness and primary stroke prevention to a wider AAPI audience.
Alice Liu – Achieving Health Equity: Recognizing the Health Profiles of Asian American and Pacific Islander (AAPI) Communities in the Greater Cleveland Area and Closing the Gap in Clinical Trials
Background: Despite clinical trials playing a crucial role in treatment development, there is significant misalignment of minority race distribution between general population and clinical trial participants in the United States. Asian Americans are one of the most underrepresented minority groups-despite being the fastest-growing population in America-constituting less than 2% of clinical trial participants. This disparity affects the generalizability of clinical trial results and equitable healthcare delivery. The aim of this study is to identify barriers to clinical trial participation specific to AAPI communities in Greater Cleveland.
Methods: This research employs a mixed-methods approach to investigate cultural and socioeconomic barriers within AAPI communities. A survey encompassing cultural and socioeconomic barriers identified in previous literature were distributed to 50 participants in each of the following communities: Chinese (Cleveland Asiatown), Chinese (Greater Cleveland Area), Filipino, Pakistani and Afghan. Qualitative data was collected through focus groups, each comprising five community members from the groups mentioned above, to facilitate comprehensive exploration of distinct obstacles experienced by each community.
Results: We collected 196 surveys, with ages of participants ranging from 19 to 89 years old. 58% of participants have heard of clinical trials, but the vast majority (92%) knew nothing or little about them. 15% have participated or knew someone who participated in a clinical trial, though 48% said they are somewhat or very likely to participate if asked. The importance of incentives such as monetary compensation, transportation, and encouragement from trusted individuals varied widely between the communities. In the focus groups, specific groups noted unique challenges stemming from cultural and religious attitudes. Key takeaways included the importance of culturally competent outreach, transparent risk disclosure and education on the benefits of clinical trials to individuals and society, and community-centered approaches to recruitment.
Conclusions: While our findings mostly align with existing literature on the common barriers to clinical trial participation for minority populations, we highlight distinct barriers and motivators within various AAPI subgroups. Further meta-analysis of demographics data and health attitudes can be used to target and address AAPI clinical trial recruitment in the Greater Cleveland area.
Sunshine Liu – Understanding Diabetes: A Comparative Analysis of Diabetes Literacy and Confidence in South Asian and White Populations in Michigan
Background: Diabetes Mellitus (DM) prevention and management remains a challenge in Michigan. As of 2023, nearly half of the state’s population is affected with DM or pre-diabetes, with higher morbidity among minority groups. To address these disparities, osteopathic medical students at Michigan State University College of Osteopathic Medicine (MSUCOM), under faculty mentorship, created Understanding Diabetes, an educational project emphasizing biomedical understanding of DM and tailored management strategies. Initially piloted in the South Asian (SA) community in Oakland County MI, it expanded to Berrien County MI, an area with higher poverty and lower educational attainment. This enabled comparisons of objective understanding and subjective confidence in managing DM between White populations of lower socioeconomic status (SES) and SA populations of higher SES.
Methods: Understanding Diabetes used an observational descriptive study design (IRB STUDY00010026), in SA (N=18) and White (N=17) populations in selected geographic areas in Michigan. Data were collected to assess the baseline objective understanding of DM across several categories as well as participant-reported confidence in managing DM. Results were analyzed by comparing populations’ proportion of correct and affirmative responses using chi-squared proportion tests (CI95).
Results: SA participants reported significantly higher confidence overall in managing DM than White participants (74% vs 51%, p<0.05). This was also seen in categories of general knowledge (86% vs 56%, p<0.05), lifestyle management (81% vs 60%, p<0.05), and complications and emergency management (68% vs 47%, p<0.05). However, regarding objective understanding, no statistically significant differences were observed between the two populations (56% vs 58%).
Conclusion: SA participants exhibited similar levels of objective understanding of DM compared to White participants despite higher SES and greater educational attainment. These findings suggest that racial factors, such as language barriers and discrimination, may influence health literacy, potentially overriding SES and education. Additionally, the higher confidence reported by SA participants may reflect underlying cultural attitudes towards DM, including stigma and tendency to act on social desirability bias. As Michigan’s SA population grows, culturally sensitive educational interventions are critical to addressing disparities and improving outcomes in this at-risk population.
Nagasriya Ramisetty – Adaptation of the Health Stigma and Discrimination Framework for Asian American Mental Health Stigma and Reported Impact on Help-Seeking Behaviors
Background: Asian Americans face the highest mental health support need of any ethnic group in the United States, but the community reports severe underutilization of available mental healthcare services. Cultural differences are a major factor that contribute to differences in the help-seeking behaviors of Asian Americans, and researchers need to delineate the unique needs of this community to adapt and establish more culturally sensitive resources and outreach methods.
Methods: We conducted a comprehensive narrative review of the Google Scholar database for research studies (n=19) that inform the relationship between Asian American mental health and different dimensions of the Health Stigma and Discrimination (HSD) Framework – drivers and facilitators of stigma, manifestations of stigma experiences and practices, outcomes for affected populations and organizations, and the health and social impacts. The HSD framework has the potential to navigate the nuances of mental healthcare need for Asian Americans as a global cross-cutting measure that identifies the various facets of health stigma and impacts on public health outreach and interventions in marginalized communities. This framework critically moves away from the binary of the “stigmatized” and “stigmatizer”, and instead identifies how stigma detrimentally affects the health outcomes of the community at large.
Results: Studies (Table 1) found that Asian Americans’ evaluation of personal mental health need fell outside of the Western model of mental health understanding, resulting in lower service usage rates despite awareness of them. Major factors affecting help-seeking behavior included fear of social judgement, different manifestations of and language regarding mental distress, shame, familial pressure, and, unique to the Asian American community, expectations of success without struggle due to internalization of the model minority myth (Figure 1).
Conclusions: This evidence defends the need for culturally sensitive mental healthcare resources that acknowledge and dismantle the internal, perceived, and experienced stigma for members of the Asian American community. We are conducting semi-structured interviews with community members and healthcare providers to better understand representations of mental distress and identify the specific barriers that limit resource usage. Future research can be applied to tailoring existing resources and outreach to improve mental health outcomes for Asian Americans.
Shivam Bhargava – Evaluating the Impact of Social Support in South Asians and Arabs with Type 2 Diabetes Through a Family-Centered Diabetes Education Program
Background: Diabetes is the fourth leading cause of death among Asians in Chicago, and the top leading cause of death among Asian Indians. Limited research investigates the role that social support plays in South Asians with Type 2 Diabetes. The All One Community Program is a diabetes management program tailored toward South Asian and Arab communities with social support aspects, adapted from existing evidence-based curricula. The program is led by Asian Health Coalition in Chicago in collaboration with three different community-based organizations that serve South Asian and Arab immigrant communities.
Materials and Methods: The program is culturally and linguistically tailored for the South Asian and Arab community and includes health literacy components related to nutrition, stress, and exercise. The program includes 13 educational sessions that are held one hour per week. Biometric data (blood pressure, BMI, and A1c) is collected at baseline, 3-months, 6-months, and 9-months. Since the launch of the program in 2022, 142 individuals have been enrolled with 87 individuals being diagnosed with Type 2 Diabetes. A survey is administered at baseline, 6-months, and 9-months that contain questions about social support related to exercise, eating, and family/friends. Social support strategies include one on one weekly check-ins with CHWs, monthly webinars with healthcare professionals, and an interactive WhatsApp group for participants to interact and support each other outside of class.
Results: 54% of participants increased their overall social support scores from the start of the program to the end 9 months later. 67% of diabetic participants increased their social support for exercise score from baseline to 9 months. Social support for eating scores increased by an average of 5.3 points for participants from baseline to 9 months. 54% of participants increased the number of days they were physically active during the week from baseline to 9 months. A total of 98.8 pounds were lost among participants from baseline to 9 months.
Conclusion: The data analyzed informs attendees about the key roles that family members, community health workers, and additional support systems play in the management of diabetes. The research also highlights that when individuals have their family members or other support system members making the same lifestyle changes that they are, it positively impacts their motivation, behavior, and habits related to their type 2 diabetes.
Elizabeth Nguyen – Asians Be Checked: Uncovering Knowledge Deficits for Hepatitis B Among Vietnamese and Filipinos in South Texas
Background: Asian Americans are disproportionately at high risk for chronic hepatitis B virus (HBV) infection. In 2021, the CDC reported that although Asian Americans comprise only 6% of the US population, they make up 60% of chronic HBV cases and are nine times more likely to die from HBV-related complications than Caucasians. Hence, we created a community advocacy project to address this disparity by providing education and promoting screening to the Asian American community.
Our community assessments reveal that among South Texas Vietnamese, over 88% reported having never been screened or being unaware of their screening status. Subsequent assessments among Chinese and Korean communities showed that over 44% of participants have never been screened for HBV. These statistics highlight disparities in hepatitis B awareness. In 2023, the CDC updated its guidelines to include universal HBV screening, emphasizing the need to bridge gaps in care. The aim of this study is to engage stakeholders by evaluating understanding of HBV among the Vietnamese and Filipinos in South Texas.
Methods: Students volunteered with Vietnamese (Lien Hoa Buddhist Temple and Vietnamese Martyrs Church) and Filipino (Philippine American Chamber of Commerce and Filipino and Pacific Islander Festival) community partners at local events. Participants responded to an online survey with the questions: 1) Are Asian Americans at higher risk for hepatitis and liver cancer? 2) Do you know what hepatitis B is? 3) Is hepatitis B preventable? 4) Is hepatitis B treatable? 5) Have you ever been screened for hepatitis B? 6) Are you interested in being screened for hepatitis B? The responses formed the basis of the education talking points, and informational flyers (Figure 1) summarizing HBV education were provided. The collected data were analyzed for descriptive statistics.
Results: Most participants (59%, n=87) did not know that Asian Americans are at higher risk for HBV. 41% lacked awareness of HBV itself and 60% were unfamiliar with chronic HBV complications, such as liver disease and cancer. 53% did not know HBV is preventable and treatable. After learning about the vaccine, 66% expressed interest in learning more and getting screened.
Conclusions: The low HBV health literacy among Vietnamese and Filipino participants underscores the need for more outreach and education. Their strong interest in screening emphasizes the importance of providing these services to address this disparity.
Eugene Oh and Hayoung Anh – Addressing Bias and Advancing Equity for AANHPI Communities in Healthcare
Background: Racism, discrimination, and bias against Asian American and Pacific Islander (AAPI) individuals persist in healthcare, creating barriers to career advancement and impacting well-being1. Despite progress in equity, diversity, and inclusion (EDI), AAPI healthcare workers face unique challenges such as being perceived as submissive, which excludes them from leadership opportunities2. At UCLA Health, concerns from AAPI community members prompted surveys to assess these issues and develop actionable solutions.
Materials & Methods: Two Qualtrics surveys were distributed to the AAPI community at UCLA Health: the first in Oct-Nov 2022 (N=127) and the second in Dec 2023-Feb 2024 (N=106). Respondents included faculty (69%), medical students (21%), staff (6%), and residents/fellows (3%). The surveys assessed experiences of racism, discrimination, and bias, and perceptions of UCLA’s response.
Results: Key findings from the 2023 survey revealed that 74% of respondents witnessed racism, discrimination, or bias against AAPI individuals (vs. 70% in 2022), and 71% personally experienced such incidents (vs. 60% in 2022). Common forms of bias included implicit bias (witnessed by 89%, experienced by 84%) and microaggressions (witnessed by 82%, experienced by 64%). Negative impacts on well-being increased to 55% (vs. 38% in 2022), and 32% considered leaving UCLA due to these experiences. Only 41% felt UCLA addressed bias effectively, and 27% felt leadership was sufficiently educated on AAPI-specific issues.
Conclusions: Despite ongoing EDI efforts, these findings highlight persistent challenges and a critical need for AAPI-specific initiatives to address bias and promote inclusion in healthcare. In response, UCLA Health has taken meaningful steps, including the recent launch of the DGSOM Center for Asian Equity and Health, which provides training for faculty, staff, and students, fosters junior faculty leadership, and lays a foundation for a supportive environment and research. A coalition of faculty and trainees is also capturing real-life stories of discrimination to create a training video raising awareness and addressing AAPI racism, now in its final stages with plans for widespread distribution. These efforts underscore the importance of systemic interventions—by implementing targeted training, encouraging open conversations, and uniting the AAPI community, academic institutions can create environments where AAPI individuals feel supported, valued, and empowered.
Anthony Trieu, Joyce Xiong, and Joanna Sung – Primary Asian Language and Risk of Hepatic Complications in Asian Americans with Chronic Hepatitis B: A Retrospective Cohort Study
Background: Chronic hepatitis B (CHB) affects Asian Americans disproportionately, yet the role of language proficiency in health outcomes remains understudied.1-2 Limited English proficiency may contribute to varied outcomes through healthcare access, communication, and treatment adherence barriers.3-4 This study investigates the impact of Asian primary language preferences on adverse outcomes in Asian Americans with CHB.
Methods: Using the TriNetX platform, we conducted a retrospective cohort study of Asian American patients diagnosed with CHB (ICD-10: B18.1), excluding those with co-infection by the hepatitis D virus (ICD-10: B18.2) and Type 2 diabetes (ICD-10: E11). Patients were stratified into two cohorts based on primary language preference: English vs. certain Asian languages (Vietnamese, Korean, or Chinese). 10-year risk of key adverse outcomes, including liver cell carcinoma (ICD-10: C22.0), fibrosis and cirrhosis of liver (ICD-10: K74), liver transplant status (ICD-10: Z94.4) and portal hypertension (ICD-10: K76.6) were analyzed across language groups. Propensity score matching was used to adjust for age and gender. Certain social factors and laboratory values to assess the severity of hepatitis could not be accounted for due to limitations to available data.
Results: Preliminary findings revealed differences in adverse outcomes based on language preference. Chinese-speaking patients demonstrated a decreased risk of adverse outcomes compared to their English-speaking counterparts, specifically in liver transplant status, cirrhosis, and portal hypertension. Vietnamese- and Korean-speaking patients exhibited a significantly higher risk of liver cell carcinoma. However, no significant differences were observed in liver transplant status, portal hypertension, or cirrhosis. Differences persisted after propensity score matching.
Conclusions: Our findings suggest that primary language preference may influence health outcomes in Asian Americans with CHB. Factors such as varied disease management education in non-English languages, cultural awareness, and public health programs domestically and/or countries of origin may contribute to different outcomes for certain groups.5-7 Future studies may explore the intersection of language proficiency, social support, and socioeconomic factors to better address disparities in CHB outcomes.
Avni Varshneya – Health Education as Harm Reduction for Clients in Addiction Recovery
Background: First Step Home (FSH) is an addiction treatment facility for people who identify as women recovering from substance use disorder (SUD). Higher levels of health knowledge and literacy can increase quality of life and mental health in this community. FSH was seeking to empower their clients through health education and learn more about the impact of a new adulterant, xylazine.
Materials and Methods: A 15-session educational course was conducted on sexual/mental health, nutrition/exercise, xylazine/harm reduction, and wound care/first aid. Pre and post-session quizzes were analyzed with a Wilcoxon signed-rank t-test to assess knowledge improvement. Gathered client feedback on health education sessions. Distributed a qualitative and quantitative survey to determine how xylazine impacts FSH residents.
Results: An average 14% increase in post-quizzes compared to the pre-quizzes was found (σ = .100, n = 8). The session on wound care and first aid showed a statistically significant improvement of 27% (p = .0312, σ = .163). Through the xylazine impact study, 28 clients were surveyed. One-third of women reported being impacted by xylazine or knowing someone else who was impacted. 50% of the clients surveyed did not know what xylazine was, and 89.3% did not know the effects of xylazine on the body or how to take care of xylazine wounds.
Conclusion: Women reported being empowered to make decisions about their healthcare and schedule reproductive health screenings after the educational course. More participants are needed to demonstrate a significant link between health education improving health knowledge for women undergoing SUD treatment. Wound care and first aid sessions showed significant increases in scores. These skills should continue to be taught because they are vital to saving the lives of people with SUD. The results of the xylazine impact survey show a striking lack of awareness about xylazine amongst clients. If clients did know what xylazine was, they often did not know about wound care or how the drug affected the body. Notably, some clients had healed wounds and only realized they may be due to xylazine as they were taking the survey. These results indicate more education is needed to equip women in addiction recovery with knowledge about harmful adulterants like xylazine, and empower them with sessions on first aid, harm reduction, and wound care techniques.
Gabriella Tran – Investigating Quality of Life Measures in Birdshot Chorioretinopathy
Background: Birdshot chorioretinopathy (BSCR) is a chronic posterior uveitis that can significantly impact visual function. Patient-reported outcomes (PROs) have gained importance in evaluating the impact of patients’ perceptions of their quality of life. This study aimed to investigate the use of psychometrically validated PRO measures, the Michigan Retinal Degeneration Questionnaire (MRDQ) and Michigan Vision-related Anxiety Questionnaire (MVAQ), for BSCR patients.
Methods: A dual-center mixed method observational study was conducted on patients with BSCR (n=21). The MRDQ and MVAQ were administered to these patients, and retrospective chart review was performed. Graded response models were fit by Cai’s Metropolis-Hastings Robbins-Monro algorithm using the R (version 3.6.3) package mirtscores for seven parameters from the MRDQ. These scores were then compared with the presence or absence of retinal vasculitis and the time between diagnosis and the most recent follow-up.
Results: Analysis of the MRDQ parameters revealed previously unrecognized patterns in visual function among birdshot chorioretinopathy (BSCR) patients. Photosensitivity with a value of 0.73 ± 1.3 and color vision with a value of 0.66 ± 0.11 were the highest scoring domains. The lowest scoring domains were mesopic peripheral function at 0.059 ± 0.09 and scotopic function 0.082 ± 0.10. A trend of retinal vasculitis impacting color vision and photosensitivity was observed. Interestingly, a significant correlation between time from diagnosis to most recent follow-up being ≥5 years and decreased photosensitivity was observed (p=0.017). MVAQ showed higher anxiety due to cone dysfunction scores, compared to rod dysfunction, further supporting that color vision is one of the most greatly impacted domains for birdshot patients.
Conclusions: The MRDQ/MVAQ results provide a previously unrecognized feature of birdshot, which is a significant impact on color vision. The domains most affected in BSCR are notably different from those reported in retinitis pigmentosa (RP). In RP, the highest observed MRDQ scores were mesopic peripheral function and contrast sensitivity, while the lowest were in photosensitivity and color vision. Both RP and BSCR affect photoreceptors, but these results indicate potential differences in pathophysiologic processes.
Hanna Suh, Sophie Lu – Investigating the Health Needs of Asiatown Community Members in Cleveland, Ohio
Background: The Asian and Pacific Islander community comprise 2.5% of Cleveland’s and 3.5% of Cuyahoga county’s population according to the 2020 census. The health needs of this community, however, are not well characterized. The aim of this study was to assess the subjective factors that affect health needs and outcomes, self-efficacy, and healthcare interactions among Cleveland’s Asiatown members.
Methods: We administered a survey to Asiatown members asking about barriers to healthcare, health literacy and transportation. Surveys were provided in English, simplified Chinese, traditional Chinese, and Korean. Responses were collected in-person at community health outreach events and online via Qualtrics. Data analyses, including t-tests with unequal variances and Fisher’s exact tests were conducted in R.
Results: We enrolled 78 participants with a mean age of 72, of which there were 60 females and 14 males (4 NA). Self-reported race was 77 Asians and 1 mixed race, with 74 Chinese, 4 Koreans, and 1 White/Chinese. The top two health concerns were blood pressure and diabetes with 36 and 19 votes respectively. 75 participants (96%) had health insurance. Most participants either drove themselves (37.2%) or were driven by others (24.4%). The primary mode of transportation of participants ages 65 and older was significantly different from those younger than 65 (p=0.002). While both groups reported driving themselves, those aged 65 and older were driven by others more often. Regarding time spent traveling to health care visits, most participants spent 10-30 minutes. Lastly, 53.8% of participants said they go to health appointments alone versus 41% who go with others (4 NA). There were no significant differences in responses based on sex.
Conclusions: Our results suggest unmet health needs of a population of elderly community members who live in Asiatown. While participants tend to have health insurance, there appear to be other barriers to health care, such as transportation insecurity and lack of social support. Limitations of this study include a small sample size as well as limited literacy in their primary language among some participants which may bias results. Future directions include tailoring future health fairs and volunteer programs to address the gaps identified in this study, such as providing transportation support.
Hao Chen – Reassessing the Healthy Immigrant Effect: Elevated Chronic Disease Prevalence Among Asian Immigrants Compared to U.S.-Born Asians
Introduction: The “healthy immigrant effect” suggests that immigrants often have better health outcomes than their native-born counterparts. This study reevaluates this concept by analyzing the prevalence of chronic diseases among Asian immigrants compared to U.S.-born Asian Americans and examining healthcare access metrics to explore potential contributors to health disparities.
Methods: Data from the Integrated Public Use Microdata Series (IPUMS) National Health Interview Survey (NHIS) was used to analyze to assess the prevalence of hypercholesterolemia, hypertension, diabetes mellitus, and cancer among individuals aged 18 and older. Foreign-born Asian immigrants were categorized by U.S. residency duration: less than one year, 1–less than 5 years, 5– less than 10 years, and more than 15 years. Healthcare access metrics, including health insurance coverage, recent doctor visits, and having a usual place of care, were also evaluated. Weighted percentages and chi-square tests were used to identify differences in prevalence and access.
Results: Among Asian immigrants, hypercholesterolemia and hypertension prevalence initially declined with longer residency—from 25.0% and 16.8% (less than one year) to 16.7% and 10.8% (5– less than 10 years)—but rose to 36.7% for both conditions after 15 years. Similarly, cancer and diabetes prevalence were 0% (less than one year), fluctuating between 1 and 15 years, and 4.6% and 15.2%, for over 15 years, respectively.
Healthcare access improved with residency duration, with insurance coverage rising from 86.3% to 97.8%, and having a usual place of care increasing from 42.6% to 91.5%. However, recent doctor visits declined (89.3% to 85.5%). Compared to U.S.-born Asians, foreign-born Asian immigrants reported higher prevalence of chronic conditions, including cancer (3.9% vs. 2.4%), hypercholesterolemia (30.6% vs. 19.6%), hypertension (29.3% vs. 16.7%), and diabetes (12.4% vs. 3.9%).
Conclusion: This study challenges the “healthy immigrant effect,” showing higher chronic disease prevalence among foreign-born Asian immigrants than U.S.-born Asians, including recent arrivals. These disparities are unlikely driven by socioeconomic barriers, as healthcare access metrics were comparable. Potential contributors include language barriers, acculturation stress, pre-existing conditions, or lifestyle changes. Future research should explore these disparities’ underlying causes and guide targeted interventions.
Himi Begum – Cervical Cancer Incidence Patterns Across Asian and Pacific Islander Populations in the U.S. (2004–2021)
Background: Cervical cancer remains a major public health issue, with significant differences in diagnosis and survival rates across racial and ethnic groups. Non-Hispanic Asian/Pacific Islander (NHAPI) women represent a diverse population, with unique challenges in accessing care and timely diagnosis. This poses a significant public health problem, given that cancer is the leading cause of death among Asian American women. This study aims to examine disparities in cervical cancer stage at diagnosis and incidence rates among API women, utilizing Surveillance, Epidemiology, and End Results (SEER) data from 2004 to 2021.
Materials and Methods: We conducted a retrospective analysis of cervical cancer cases recorded in the SEER*Stat database from 2004 to 2021. Data were stratified by race and ethnicity, focusing on specific NHAPI subgroups (e.g., Vietnamese, Korean, Japanese, Chinese, Filipino). We compared stage at diagnosis (i.e., Localized, Regional, Distant), age-adjusted incidence rates, and mortality rates between NHAPI subgroups and non-Hispanic White women.
Results: Overall, the 5-year cervical cancer incidence rates for NHAPI women were generally lower than those for non-Hispanic White women, except for Native Hawaiian women (6.1 per 100,000 vs. 6.9 per 100,000). The 5-year age-adjusted mortality rates were lower for NHAPI women compared to non-Hispanic White women (1.6 per 100,000 vs. 2.1 per 100,000). In general, certain API groups had less favorable distributions of stage at diagnosis compared to non-Hispanic White women. Among stratified NHAPI subgroups, Chinese and Filipino women had the highest rates of late-stage cervical cancer diagnoses.
Conclusions: This study highlights disparities in cervical cancer incidence and stage at diagnosis between specific NHAPI subgroups and non-Hispanic White women. The higher rates of late-stage diagnoses among Chinese and Filipino women underscore the need for targeted cancer prevention measures. These findings demonstrate the importance of understanding the unique health challenges across NHAPI groups to improve outcomes.
Isabel Kilroy – Built Environment and Housing Quality on Mental Health Outcomes Among Filipinos in the HoPES Cohort
Background: The rising prevalence of mental health issues is a global public health concern. A social determinants approach to mental health highlights that the conditions in which individuals live, work, and grow shape mental health outcomes. Housing is a cardinal social determinant of health, and recent research has emphasized the impact of the built environment (including housing quality and urban design) on well-being. The Philippines, ranked third in mental illness prevalence in the Western Pacific, faces a housing crisis worsened by socioeconomic inequality and climate disaster. Thus, exploring the impact of the built environment on Filipino mental health is crucial. Filipino Americans comprise the 3rd largest Asian ethnic subgroup in the U.S., and Asians are projected to be the largest immigrant group in the U.S. by 2055. Within this community, mental health stigma and cultural values often discourage formal help-seeking, despite high rates of psychological distress. Therefore, identifying “upstream factors” such as housing and the built environment is critical to addressing the mental health needs of Filipino Americans and AANHPI more broadly. Materials and
Methods: We conducted a secondary analysis of baseline data from the non-migrant sample of the Health of Philippine Emigrants Study (HoPES; n=805). Using multiple linear regression and logistic regression analyses, we examined the association between built environment quality and depressive symptoms, and the impact of built environment quality on substance use, specifically cigarette use and binge drinking.
Results: Overall, poor quality built environment was significantly associated with greater depressive symptoms (β = 0.079, p = 0.013) and smoking (β = 0.13, p = 0.0013), but not binge drinking (β = -0.058, p = 0.115) after adjusting for covariates.
Conclusion: Clinicians across all specialties play a key role in recognizing the impact of housing quality and the built environment on mental health. Integrating this awareness into medical training, incorporating questions on built environment within clinical assessment, and fostering interdisciplinary collaboration, especially with public health and social work fields, are essential steps to addressing the impact of built environment on mental health outcomes in the Filipino community. Ultimately, advocating for healthier policies that improve the conditions in which patients live, work, and grow is vital to optimizing community health outcomes.
Rachel Prince – The Role of Asian Culture and Language in Diabetes and Vision Care
Background: Asians face high rates of diabetes and diabetic retinopathy (DR) and have disproportionately low diabetes screening rates but are underrepresented in vision research, with distinct ethnicities often aggregated. We investigated the role of language and cultural preferences in shaping the understanding and management of diabetes and eye care by analyzing perspectives across Asian subgroups.
Methods: We conducted virtual semi-structured interviews with a purposive sample of Asian-identifying, English-speaking adults with diabetes residing in Connecticut. We created an interview guide based on our DR determinants framework. All interviews were transcribed and analyzed using NVivo software. We conducted consensus-based coding and both deductive and inductive thematic analysis until we achieved thematic saturation.
Results: We recruited 10 participants with diabetes (median age 65.9 years, 60% female) of Chinese, Filipino, Indian, and Vietnamese ethnicities. We identified 27 concepts under eight themes: cues to action, cultural understanding, diabetes management, health awareness, knowledge-creating experiences, patient education, physician-patient interaction, and vision status. Over half the participants stated they were not made aware of the link between eye health and diabetes or the rationale behind diabetic eye exams. Participants preferred providers of similar ethnicities due to a shared understanding of diet, lifestyle, and language, which improved comprehension and management of their health conditions. They also cited diet, lifestyle, and cultural beliefs as key challenges of managing diabetes, emphasizing the need for cultural integration into health management plans. Participants also generated ideas for improved communication with patients with limited English proficiency. While the original framework examined broad factors influencing DR screening, our study focused on cultural and linguistic influences on diabetes and eye health in Asians.
Conclusions: Participants recognize the need for cultural understanding from providers, especially in regard to patient education and diabetes management. It is crucial to develop interventions tailored to Asian communities that emphasize the link between diabetes and eye health and address cultural and language barriers.
Sandhya Sewnauth – The Impact of Colonialism on Present-Day Indo-Caribbean Health
Background: Indo-Caribbeans are currently the fifth largest immigrant group in New York City, and the second largest immigrant population in the borough of Queens. There are several significant health disparities that exist within this community, including elevated rates of cardiovascular disease, diabetes, and binge drinking. To develop culturally appropriate and trauma-informed strategies to address this, we need to understand the complex historical factors that led to disproportionate health outcomes. By analyzing colonialism as a social determinant of health, we can create sustainable healthcare improvements within this under-researched population of the South Asian diaspora.
Methods: Existing literature on present-day health disparities was assessed using PubMed and Research Open World databases. A community health resources and needs assessment conducted by the NYU Center for the Study of Asian American Health from 2013-2015 was also consulted. Primary sources from the colonial period were accessed at the British Library in London, UK.
Results: The Indian indenture system contributed to several health disparities in the Indo-Caribbean population. This includes the cardiometabolic effects of colonial-driven famines that devastated the regions of India where the majority of indentured laborers were recruited. The economy in the Caribbean colonies focused solely on sugar cultivation, which influenced the diet and lifestyle of this population, including the high number of distilleries in their communities. The experiences of working as indentured laborers also led to mental health crises, including suicidal ideation, and generational trauma among the diaspora.
Conclusions: The health of Indo-Caribbean immigrants is uniquely affected by the legacy of the indentured laborer system during British colonial rule. These results will inform a culturally appropriate and trauma-informed resource guide that focuses on the topics of cardiovascular disease, diabetes, alcohol use disorder, and mental health. While more research is needed on present-day health disparities within this population, tailored resource guides will empower community members to tackle negative health outcomes, enabling future generations to thrive.
Arion Yu – The acute effects of alpha-lactalbumin intake on tryptophan metabolites and mood in older adults with Mild Cognitive Impairment
Background: Mild Cognitive Impairment (MCI) represents a transitional stage between normal cognitive aging and more severe neurodegenerative disorders in the elderly such as Alzheimer’s Disease. MCI is often accompanied by depressed mood and other mood disturbances which can obfuscate what is causing declining cognition. Serotonin (5-HT), a neurotransmitter involved in regulating mood, is synthesized from the essential amino acid tryptophan. Availability of serotonin is largely influenced by the metabolism of tryptophan through either the serotonin or kynurenine pathway. This manuscript explores the potential relationship between MCI, depressed mood, and tryptophan metabolism in the elderly, with a particular focus on the effects of a tryptophan-rich dietary intervention. We first examine the differences in tryptophan metabolism between MCI elderly adults and healthy older adults at baseline. Subsequently, we examine how intake of alpha-lactalbumin (ALAC), a protein rich in tryptophan, affects tryptophan metabolism and if it could serve as an effective strategy for enhancing mood in older adults with mild cognitive impairment.
Methods: 32 older adults (age 55 and up) with MCI and 26 older adults matched for age, sex, and BMI without MCI participated in this cross sectional study. Serum tryptophan metabolites at baseline were measured. A smaller subset of these subjects then consumed a meal enriched with ALAC. Plasma tryptophan metabolites after introduction of the meal were measured and changes in mood were assessed before and after meal intake.
Results: MCI subjects had higher levels of plasma anthranilic acid at baseline. Intake of ALAC resulted in an increase in plasma tryptophan (TRP), kynurenine (KYN) , 3-hydroxykynurenine (3-HK), anthranilic acid (AA), kynurenic acid (KYNA), and picolinic acid (PICO). There were no differences in 5-HT before and after ALAC intake. Additionally, there was a MCI interaction with picolinic acid. The TRP/LNAA ratio increased by 89.9% in MCI subjects and 95.9% in controls. There were no acute changes in mood before and after ALAC intake.
Conclusions: Elderly adults with MCI have different tryptophan metabolism down the kynurenine pathway. Consumption of a dietary protein rich in tryptophan increases metabolites of the kynurenine pathway as well as the TRP/LNAA ratio. The ALAC protein had no effect on mood.
Brandon Deguzman – Underdiagnosis of Trauma and PTSD in a Low-Income, Minority-Predominant Outpatient Setting: A Comparison of Self-Assessments and Medical Records
Background: Posttraumatic stress disorder (PTSD) is a debilitating psychiatric condition that can result from traumatic events. It is characterized by intrusive thoughts, avoidance, and mood changes, and often complicated by several common comorbidities, including major depression and substance use disorders. PTSD has a lifetime prevalence of 9.4% in the United States but is often under- or mis-diagnosed. Several validated screening tools and structured assessments exist to detect trauma and PTSD, but their efficacy has not been well studied in low income, inner-city outpatient settings, in which trauma tends to be highly prevalent. The current study evaluated if validated self-report measures would capture the prevalence and trauma elements of PTSD more accurately than standard clinical interviews. The study characterized the demographics of an inner-city outpatient population, PTSD prevalence, comorbidities, and treatment.
Materials and Methods: A survey was conducted of 100 adult outpatients being treated at a large inner-city psychiatric clinic. This clinic provides safety-net services for an otherwise unserved, mostly minority population in Los Angeles County. Each participant completed two self-report measures: Life Events Checklist for DSM-5-Extended (LEC-5) and the PTSD Checklist for DSM-5 (PCL-5). Patient responses to the measures were then compared to corresponding data extracted from a medical chart review.
Results: Of the 100 participants, 50 were male, 50 were female, 66 self-identified as Latine/x, and 79 were unmarried. Physical assault (60%), transportation accidents (57%), and other unwanted sexual experiences (47%) were the most frequently reported traumas. The most commonly endorsed symptoms were feeling upset when reminded of the trauma (68%), insomnia (68%), and difficulty concentrating (66%). 56 participants met criteria for a provisional DSM-5 PTSD diagnosis, but only 29 indicated a PTSD diagnosis in their medical records. The PCL-5 and the medical record demonstrated fair agreement in PTSD diagnosis (Kappa = 0.219; SE of kappa = 0.082). A significant difference was found between the LEC-5 and the medical record in capturing the number of trauma event categories endorsed by participants (t(99) = 13.1834, p < .0001).
Conclusions: PTSD may be underdiagnosed in outpatient settings. Implementing validated self-report trauma screening measures may improve identification and treatment of PTSD among historically underserved populations.
John Huang – Evaluating Diurnal Responses to Timolol and Latanoprost from iCare HOME Intraocular Pressure Data
Background: Current glaucoma management relies on trial-and error with intraocular pressure (IOP) measured only during office hours. This limits our understanding of drug responses over a diurnal period. iCare HOME, a self-tonometer, may address this issue. This study examined timolol and latanoprost responders using diurnal IOP data from iCare HOME via cosinor rhythmometry.
Methods: Forty-seven subjects (22 male, mean age 61±9 years) with ocular hypertension or open-angle glaucoma, were enrolled in a randomized, crossover trial of latanoprost and timolol. IOP was measured using pneumatonometry and iCare IC200 at 3 of 6 study visits: baseline, after 1 week of first treatment, and after 1 week of second treatment. Subjects measured their IOP with iCare HOME at least 6 times daily for 1 week before visits. Eyes were labeled responders to timolol or latanoprost if IOP decreased ≥15% from baseline. Diurnal IOP data were analyzed and modeled with cosinor rhythmometry using R (Figure 1).
Results: For timolol, iCare HOME and pneumatonometry identified the same eye as a responder or non-responder in 60.4% of eyes (n=53). For latanoprost, the two tonometers agreed in 69.6% of eyes (n=56). Agreement between iCare HOME and iCare IC200 occurred in 54.5% of eyes (n=55) for timolol and 62.1% of eyes (n=58) for latanoprost (Figure 2). The chi-squared test for independence revealed that classifications of latanoprost responders between iCare HOME and the clinic tonometers, pneumatonometry (p=0.0025) and iCare IC200 (p=0.0137), were significantly different. No such difference was found with timolol responder classification.
Conclusions: When determining timolol responders, home and clinic tonometers show comparable classifications. For latanoprost, significant differences in classifications highlight discrepancies between home and clinic tonometry, suggesting that incorporating 24-hour monitoring may impact classifications. iCare HOME may improve glaucoma management by capturing IOP fluctuations to better identify responders.
Juben Angelo Saez – The angiotensin (1-7) glycopeptide PNA5 reduces cognitive dysfunction in a chronic progressive mouse model of Parkinson’s disease through modulation of neuroinflammation
Parkinson Disease (PD) is a widespread disease, however treatment primarily focuses on resolution of motor symptoms with currently no therapeutics that aim to accurately improve cognitive decline associated with PD. It has been shown in previous studies that MAS receptor agonism via glycosylated angiotensin (1-7) peptide, PNA5, effectively reduces cognitive decline in models of vascular contributions to cognitive impairment and dementia (VCID). The two goals of this study were to determine if systemic administration of PNA5 decreased cognitive decline in a PD mouse model and to determine if improved cognitive status can be correlated to histopathological or blood-plasma changes. Mice over-expressing human, wild-type α-synuclein (αSyn) under the Thy1 promoter (Thy1-αSyn- mice), were used as a model of PD with cognitive decline. Beginning at 4 months of age, Thy1-αSyn mice were treated with a systemic dose of PNA5 or saline solution (1 mg/kg/day). Thy1-αSyn mice then underwent behavioral testing at 6 months of age which included Y-maze, nest building, open field test, novel object recognition, and challenging beam test. Thy1-αSyn- mice were compared with wild-type mice treated with saline. Mice brains were then analyzed for changes to brain pathology using immunohistochemistry, microscopy and image analysis, stereology, Western blot, and plasma collection and immunoassay. Treatment with PNA5 reversed cognitive dysfunction measured by Novel Object Recognition and spontaneous alteration in a Y-maze in Thy1-αSyn mice. PNA5 treatment was specific to cognitive deficits as the number of errors per step on the challenging beam and nestlet building test did not change between Thy1-αSyn mice and WT. With analysis of brain tissue, enhanced cognition was associated with decreases in hippocampal inflammation and reductions in circulating levels of Macrophage Induced Protein (MIP-1β), a chemokine implicated in cognitive decline. Neuronal loss was also blunted within the CA3 hippocampal region of PNA5-treated αsyn mice. This data reveals that PNA5 treatment reduces cognitive dysfunction in a mouse model of PD and that MIP-1β can be used as a candidate biomarker for future target engagement.
Liana Ysabel Bautista – Pain Perception in Patients with Comorbid Fibromyalgia, ADHD and Obstructive Sleep Apnea Undergoing Treatment with Continuous Positive Airway Pressure: A Cross-Sectional Study
Background: Fibromyalgia (FM) is a syndrome of chronic widespread musculoskeletal pain with serious adverse health and economic outcomes (1,2). FM is not well understood, but ongoing research suggests that it is a disorder of pain regulation. It is specifically thought that central sensitization results in pain hypersensitivity. Patients experience chronic pain in the absence of musculoskeletal inflammation and structural damage (3). Moreover, there is a high frequency of ADHD symptoms and diagnosis among patients with FM, and improvement in sleep may improve not only pain but also executive function (4). For some patients with ADHD, symptoms are worsened by sleep disturbance due to OSA, and symptoms are markedly improved with appropriate treatment of obstructive sleep apnea (OSA) (5). Because sleep (and especially REM sleep) deprivation increases central sensitization, it stands to reason that for patients with FM and OSA, appropriate treatment of OSA will lead to improvement in pain perception and neuropsychiatric sequelae (5-9).
Aims: Examine the relationship of pain perception between three commonly comorbid disorders: Fibromyalgia (FM), Obstructive Sleep Apnea (OSA), and Attention Deficit/Hyperactivity Disorder (ADHD). We specifically aim to examine the effect of CPAP treatment on attention in patients with comorbid FM and OSA
Methods: After IRB approval, FM patients with OSA were identified. After written informed consent, ASRS-v1.1 was administered to FM patients seen at Loyola Outpatient center. McGill Pain Questionnaire (MPQ) 11 was administered. We analyzed sleep studies and divided the FM patients into 3 groups 1.Mild OSA 2. Moderate OSA 3. Severe OSA based on apnea/hypopnea index (AHI). We then identified OSA patients undergoing CPAP treatment and analyzed their ASRS score and compared ASRS score to non CPAP patients. REM rebound scores were analyzed.
Results: With MPQ of +25 signifying severe pain.
ADHD positive n = 24
ADHD positive and Severe MPQ Score n= 16 MPQ mean score ADHD positive: 27.67 ADHD CPAP Compliance: 44%
ADHD negative n = 26
ADHD positive and Severe MPQ Score n = 7 MPQ mean score ADHD negative: 19.23 ADHD CPAP Compliance: 55%
Conclusion: Findings show that there is a correlation between a positive ADHD diagnosis and having a more severe pain perception regarding FM symptoms. With regards to CPAP compliance, which could be influencing pain perception in these patients, we saw the ADHD positive group was less compliant.
Manav Jain – Assessment of Plasma Tetrahydrobiopterin (BH4) Levels in Individuals with Multiple Sclerosis: An Exploratory Study
Background: Multiple sclerosis (MS) is a complex neurological disease with varied clinical presentations. Oxidative stress is a key contributor to MS pathogenesis, characterized by the overproduction of reactive oxygen and nitrogen species, resulting in neurotoxicity and disease progression. Tetrahydrobiopterin (BH4), a cofactor for nitric oxide synthase, is vital for redox homeostasis. BH4 depletion amplifies oxidative stress, disrupting nitric oxide synthesis. Prior research indicates that reduced BH4 levels correlate with oxidative stress-related pathologies. This study investigates BH4 as a potential non-invasive biomarker for MS diagnosis, hypothesizing lower BH4 levels in MS patients compared to healthy controls.
Materials and Methods: This proof-of-concept study recruited MS patients (relapsing-remitting MS [RRMS], secondary-progressive MS [SPMS], primary-progressive MS [PPMS], and clinically isolated syndrome [CIS]) and healthy controls. Inclusion criteria were ages 18–40, BMI <28.5, ambulatory status (EDSS <3.5), and informed consent. Exclusions included significant systemic diseases, pregnancy, and recent smoking or medication use. Plasma BH4 levels were quantified via liquid chromatography-mass spectrometry (LC-MS). Stabilization agents included dithiothreitol, ascorbic acid, and trichloroacetic acid. Samples were centrifuged, snap-frozen, and stored at −80°C. Statistical analyses employed independent t-tests or Mann-Whitney U tests for non-normal data.
Results: Pilot data from 20 plasma samples revealed reduced BH4 levels in MS patients (6 ± 2 ng/mL) compared to controls (7.7 ± 2 ng/mL, p < 0.01, Cohen’s d). Reduced BH4 levels were observed in young, mobile RRMS patients with mild disability (EDSS <3.5), stable disease, no comorbidities, and no smoking or excessive alcohol use. Participants were predominantly on high-efficacy disease-modifying therapies.
Conclusions: Preliminary findings highlight BH4’s potential as a sensitive biomarker for oxidative stress in MS, independent of clinical stability or radiological findings. This study underscores the importance of integrating molecular biomarkers like BH4 with traditional markers (e.g., MRI, neurofilaments, GFAP) to enhance MS management and individualized treatment strategies. Ongoing recruitment aims to validate these findings across diverse MS phenotypes.
Charles Guo – Suppression of Integrin-Linked Kinase Inhibits SPARC’s Effect on Extracellular Matrix and Intraocular Pressure
Background: Primary open-angle glaucoma is a progressive eye disease where aqueous humor is inadequately drained from the trabecular meshwork (TM). While the exact mechanism is still unknown, Secreted Protein, Acidic and Rich in Cysteine (SPARC) is shown to be a key regulator of extracellular matrix (ECM) proteins that elevate intraocular pressure (IOP). Integrin-Linked Kinase (ILK) is a membrane-bound kinase shown to interact with SPARC and also regulate the ECM. We overexpressed SPARC and then inhibited ILK in mice and human models to investigate the pathway of how SPARC regulates ECM proteins in the trabecular meshwork (TM). We hypothesize that SPARC mediates its effect through ILK.
Materials and Methods: Live mice eyes, human cadaveric anterior segments, and primary human TM cells were treated with an adenovirus carrying cDNA of human SPARC (Ad.SPARC) causing overexpression and a lentivirus carrying shRNA targeting ILK (shILK) to inhibit ILK. IOP measurements were performed on live mice eyes and human anterior segments. TM cells were analyzed by immunoblotting and immunostaining. Statistical analysis was performed in Prism.
Results: SPARC overexpression in mice increased IOP compared to baseline by 1.61±0.94mmHg (p=0.047, n=10). Subsequent shRNA-mediated ILK inhibition reduced IOP by 3.51±0.92mmHg (p=0.009, n=8) compared to SPARC overexpression. In human anterior segments, SPARC overexpression elevated IOP 2.10±0.25fold (p=0.021, n=4), however, addition of shILK attenuated SPARC’s effect and decreased IOP 0.61±0.31fold (p=0.015, n=4). In human TM cells, SPARC overexpression increased levels 3.2±2.5fold (p=0.029, n=12) and also induced elevated laminin 1.45±0.37fold (p=0.004, n=10) compared to controls. ILK inhibition reduced levels 0.54±0.17fold (p<0.001, n=12) and also reduced levels of collagen I 0.60±0.17fold (p<0.001, n=8) and collagen VI 0.67±0.17fold (p<0.001, n=8).
Conclusions: ILK inhibition by shRNA attenuated the effects of SPARC overexpression on IOP and ECM proteins, implicating ILK signaling as a major molecular pathway of SPARC-mediated regulation of ECM homeostasis in TM. ILK is important in the downstream cascade of SPARC.
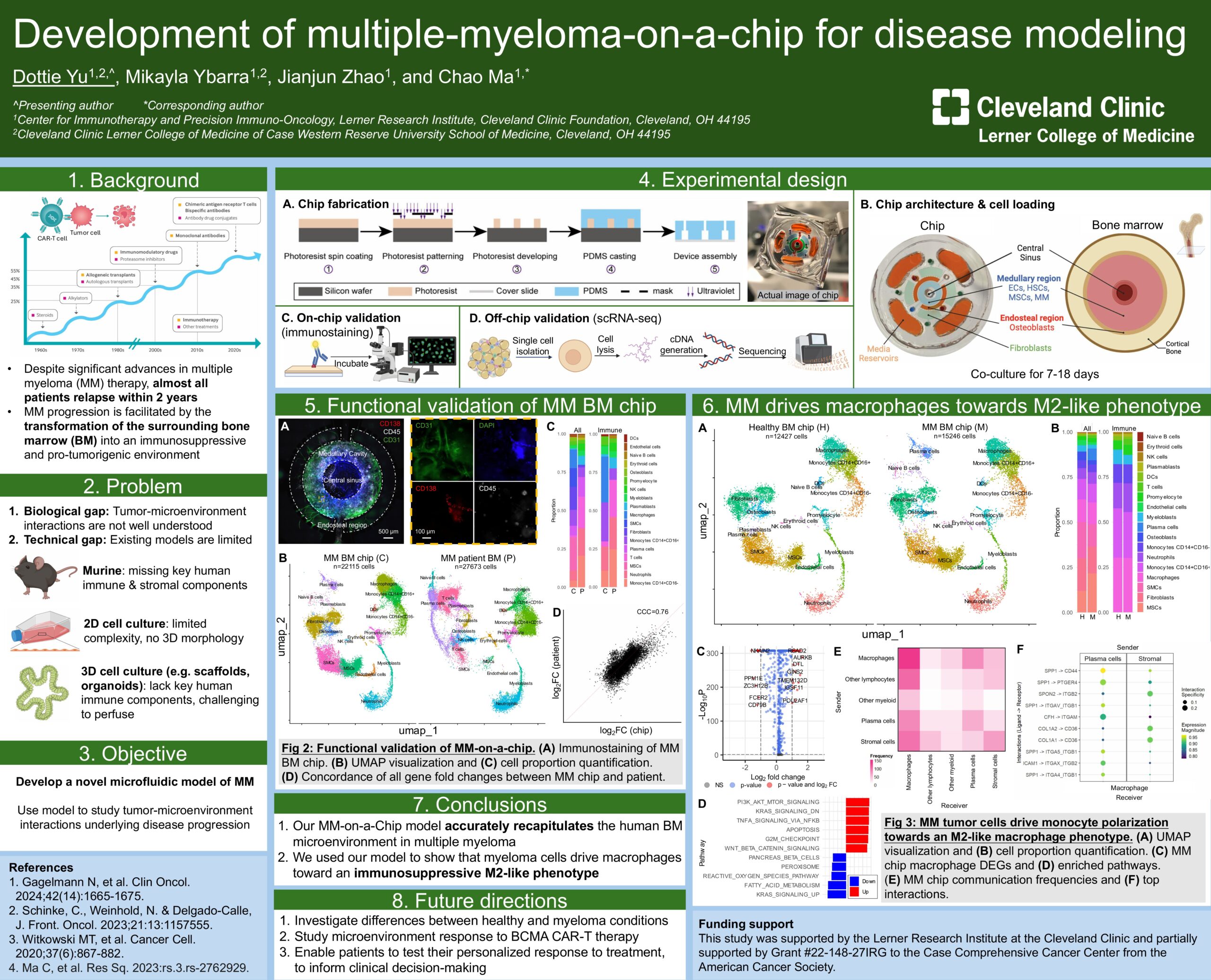
Dottie Yu – Development of Multiple Myeloma-on-a-Chip for Disease Modeling
Background: A hallmark of multiple myeloma (MM) is the transformation of the bone marrow (BM) microenvironment into an immunosuppressive niche that supports the migration, proliferation, and survival of malignant cells[1–3]. Preclinical murine models and 2D/3D cell culture systems are commonly used to study MM; however, they can be limited in fully capturing the complexity of the tumor microenvironment in a human context[4]. As such, there is a need for an ex-vivo model that most accurately recapitulates the immune and stromal components of the human BM environment, especially for testing CAR T-Cell therapy.
Materials and Methods: To emulate the microarchitecture of the BM, we designed the chip with concentric chambers representing the central sinus (central inlet), medullary cavity (inner chamber), and endosteal region (middle chamber) of the bone marrow. Chips are fabricated using replica molding technique by casting polydimethylsiloxane onto silicon wafer molds, followed by hole-punching inlets and outlets, bonding onto glass coverslips, and UV sterilization. To recreate the cellular composition of the BM, we seeded the chambers with human multiple myeloma blasts, primary human umbilical endothelial cells, primary human mesenchymal stem cells, osteoblasts, and fibroblasts. The chips were cultured for 1 week and characterized by immunostaining of vessel, immune and multiple myeloma markers.
Results: Our model demonstrated key features of the BM tissue in MM, with evidence of vascularization and MM cell localization in the medullary cavity region (inner chamber). Validation was further supported by integrating scRNA-seq data from 22115 healthy, new diagnosis, and relapse MM cells. We classified the cells into 8 immune cell types and found distinct changes in gene expression between the relapse samples compared to the healthy and new diagnosis ones. We are now investigating the role of these genes in MM progression and treatment resistance in CAR T-cell therapy using our MM-on-a-Chip.
Conclusion: The MM-on-a-Chip emulates key features of the BM environment in MM and provides a novel platform for studying the cellular interactions and microenvironment evolution in disease progression. Integrating this model with scRNA-seq analysis will build on our current understanding of the immune niche in MM progression and serve as a promising avenue for preclinical testing of novel therapies.