Tracy Gao, Network Director

Network Director
Hi everyone! My name is Tracy Gao, and I am a medical student at Sidney Kimmel Medical College at Thomas Jefferson University. I joined APAMSA at SKMC during my first year of medical school as the community service and advocacy director, and served as a Region 3 co-director for two years. This year, I am excited to be serving as the Network Director for National APAMSA. I attended Johns Hopkins University for undergrad and studied anthropology and women, gender, and sexuality studies. After college, I worked at Womankind before medical school as a residential advocate, providing counseling and case management services to survivors of gender based violence in the Asian-American, Immigrant, and other marginalized communities in New York City. My research interests include intimate partner violence, trauma-informed care, and pregnancy screening. Outside of school, I enjoy pottery, photography, graphic design, flower arranging, gardening and building new rooms for my kitten’s cardboard castle.
Statement on the Historic Confirmation of Judge Ketanji Brown Jackson
On April 7th, 2022, Judge Ketanji Brown Jackson was confirmed to the US Supreme Court as the first Black woman, the second woman of color, and the third Black Justice in its 232-year history. APAMSA celebrates this monumental moment as the next step in building an increasingly inclusive society with greater representation of people of color in positions of power.
Supreme Court Justice Jackson is one of many stepping stones for all minority communities. This is especially true when the issues important to communities of color, including that of AANHPI communities, are being decided. In particular, we renew our call for increased representation in the positions of prominence within medicine and academia. The diversity of our doctors must continue to grow for the sake of our minority communities, and our leadership is even more wanting for proper representation. We find hope in the current progress and are eager to see the path continue toward a more inclusive, just, and equitable society.
For questions or concerns about this statement, please reach out to Eric rapidresponse@apamsa.org
Statement on the Brooklyn Shooting
On the morning of April 12th, 2022, a man opened fire on the passengers of a subway train in Brooklyn, New York and ultimately injured 17 people before fleeing the scene. We at APAMSA grieve for the victims and acknowledge the fear that now strikes many New Yorkers’ hearts. We continue to denounce gun violence and reaffirm our support for comprehensive gun reform that would promote the health and safety of our communities. National APAMSA offers its support to all local chapters and its members during these frightening times, and we encourage you to reach out with any specific ways we can be of service.
For questions or concerns about this statement, please reach out to Eric rapidresponse@apamsa.org
If you are interested in exploring additional ways APAMSA can lend our support during these trying times, please reach out to Nathan at mentalhealth@apamsa.org, or the Region 2 Directors at region2@apamsa.org
Let's Talk About Sex (Education)
Let’s talk about sex (education)! Join us as we hear about advocating for sex education in the South Asian community from Nawal Umar. They are a policy analyst at SIECUS: Sex Ed for Social Change.
Zoom meeting Meeting ID: 912 5703 5311. Passcode: Health1.
Please submit any topics or questions you would like our speaker to discuss by April 14th https://forms.gle/s88AfTdoeJq9utjx8. Email any questions to email Aliasger Ezzi at sadirector@apamsa.org.
Leena Yin, MD

Network Director
Leena Yin served as Advocacy Vice President from 2020-2022, overseeing APAMSA’s response to the start of the COVID pandemic, the rise in anti-Asian hate crimes, and the resurgence of the #BlackLivesMatter movement. She completed undergrad at Stanford and medical school at the University of California, San Francisco, and will next be moving to work with AANHPI communities in Seattle as a Family Medicine resident of Swedish Cherry Hill. Leena is passionate about political organizing, her cats, and boba.
Radiology Bootcamp
Come join APAMSA on Sunday April 3rd from 4PM-6PM EST (1PM-3PM PST) for our Radiology Bootcamp! Perfect preparation for a sub-I or intern year. Our residents will be covering all the high yield topics you will need to be successful, including premedication, basics of chest and abdominal radiographs, and common indications for imaging studies. Register at: https://bit.ly/3HWsi7K
ACA & AANHPI Health with Dr. Howard Koh
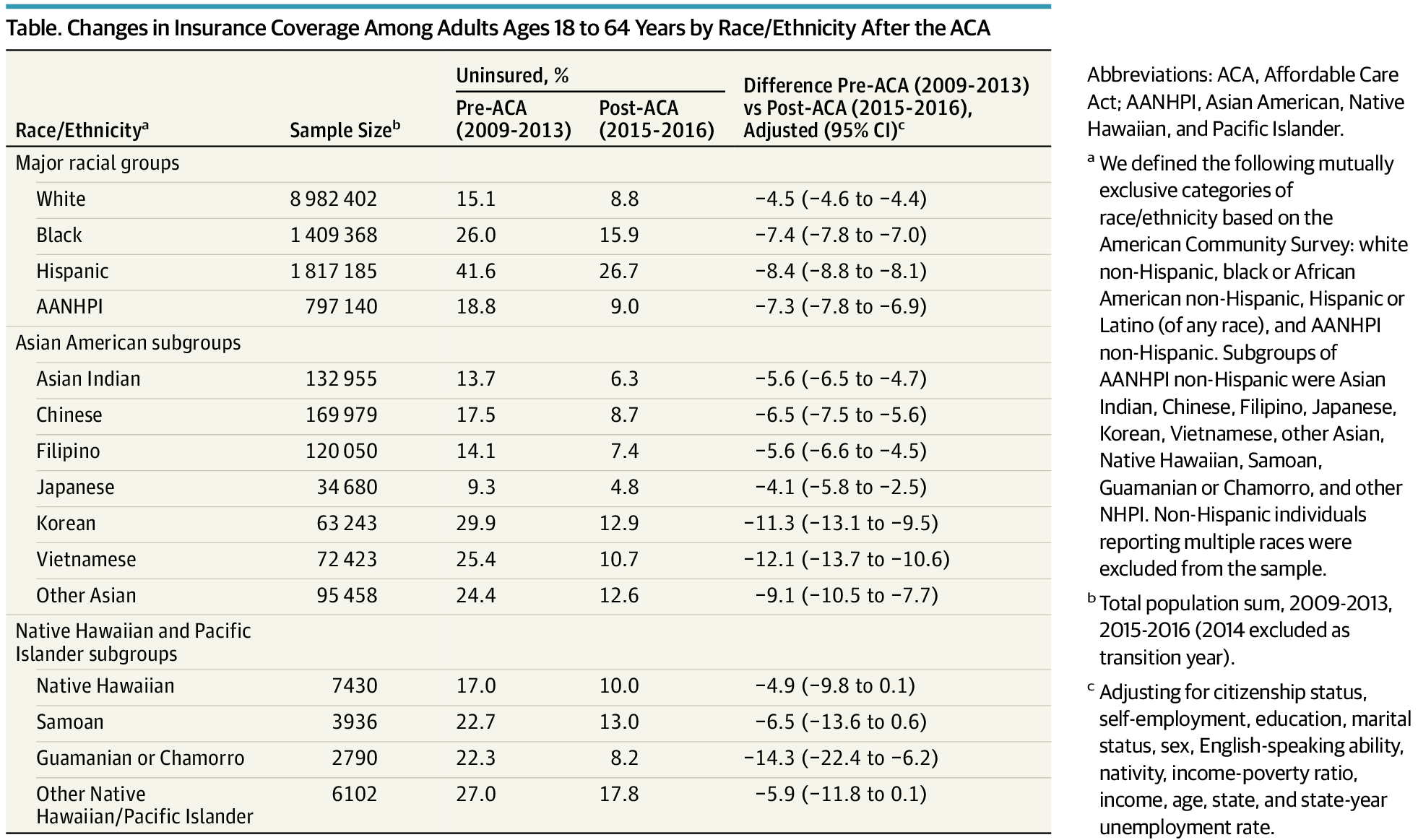
Did you know? The Affordable Care Act (ACA) halved the AANHPI uninsured rate.
Why do I need to care today? 3 million Americans will lose coverage at the end of 2022 if expanded subsidies expire.
How do I learn more? Come to our Zoom webinar with Dr. Howard Koh, former Assistant Secretary of Health in the Obama administration, this Wednesday at 1:30pm ET/10:30am PT. Registration here: https://harvard.zoom.us/webinar/register/WN_sPqUQkSuSRaZexrysZWdNQ
The ACA was signed into law in 2010. Dr. Koh will talk about some of the major benefits the law has brought in reducing the uninsured rate for AANHPI communities. Still, 30 million Americans remain uninsured today. The American Rescue Plan Act (ARPA) passed in 2021 expanded subsidies to help patients buy health insurance on the ACA exchange. But, this critical support is due to expire at the end of 2022 unless Congress takes action. APAMSA will focus this webinar on understanding why the ACA is so important for our community and why we should be activated to fight for public policy that brings us closer to (and not further away from) universal healthcare coverage.
Psychiatry Bootcamp
Come join APAMSA on Thursday March 31st from 7PM-8PM EST (4PM-5PM PST) for our Psychiatry Bootcamp! Perfect preparation for a sub-I or intern year. Our residents will be covering all the high yield topics you will need to be successful, including safety and mental status assessment, agitation, acute dystonia, PRN medications, and capacity. Register at: https://bit.ly/3sNyB92
Psychiatry Bootcamp
Come join APAMSA on Thursday March 31st from 7PM-8PM EST (4PM-5PM PST) for our Psychiatry Bootcamp! Perfect preparation for a sub-I or intern year. Our residents will be covering all the high yield topics you will need to be successful, including safety and mental status assessment, agitation, acute dystonia, PRN medications, and capacity. Register at: https://bit.ly/3sNyB92
ACA 12 Years Later: Impact on AANHPI Communities
Twelve years ago on March 23, 2010, the Patient Protection and Affordable Care Act (ACA) was signed into law by President Barack Obama. The expansive law included provisions such as an expansion of Medicaid eligibility and the introduction of a health insurance marketplace with federal subsidies to help low-income Americans afford health insurance. Since then, the uninsured rate among non-elderly adults has fallen nearly 40% from 17.8% in 2010 to 10.9% in 2019 according to analyses by the Kaiser Family Foundation.
During this weeklong celebration of the ACA hosted by The White House and the Department of Health and Human Services, APAMSA highlights the impact of the ACA on the AANHPI communities. In a 2018 publication by John J. Park et al. in JAMA Internal Medicine, the authors found that the AANHPI uninsured rate fell by more than one half from 18.8% before the ACA to 9.0% by 2015-2016. In particular, the study examined differences by AANHPI subgroup. Korean Americans, who had the highest pre-ACA uninsured rate at 29.9%, saw their uninsured rate fall an adjusted 11.3 percentage points. Guamanian or Chamorro Americans saw a 14.3 percentage point adjusted reduction in their uninsured rate. In context, the ACA nearly eliminated the coverage gap between white and ANHPI Americans. Still, 7.4% of AANHPIs remained uninsured as of 2019 with uninsured rates for other race and ethnic groups as high as 20% for Hispanic Americans. Thus, the ACA may have significantly reduced the coverage gap, but it is clear that substantial work remains to achieve universal equitable health coverage for AANHPI communities and all Americans — a goal APAMSA remains steadfastly committed to realizing in our advocacy.